How College Athletics Is Bracing for Its Latest Battle With Omicron, COVID-19

We're about to enter 2022. But it's recently started to feel a lot like 2020 to UCLA athletic director Martin Jarmond.
He is presiding over a department that is conducting several rounds of contact tracing per day. He is checking daily on his teams’ roster availability numbers. And he’s walking into locker rooms to deliver grim news about a game cancellation.
“It is a bit of a déjà vu,” Jarmond says. “It’s a, ‘Here we go again!’ It’s not a good feeling. No one is sleeping well.”
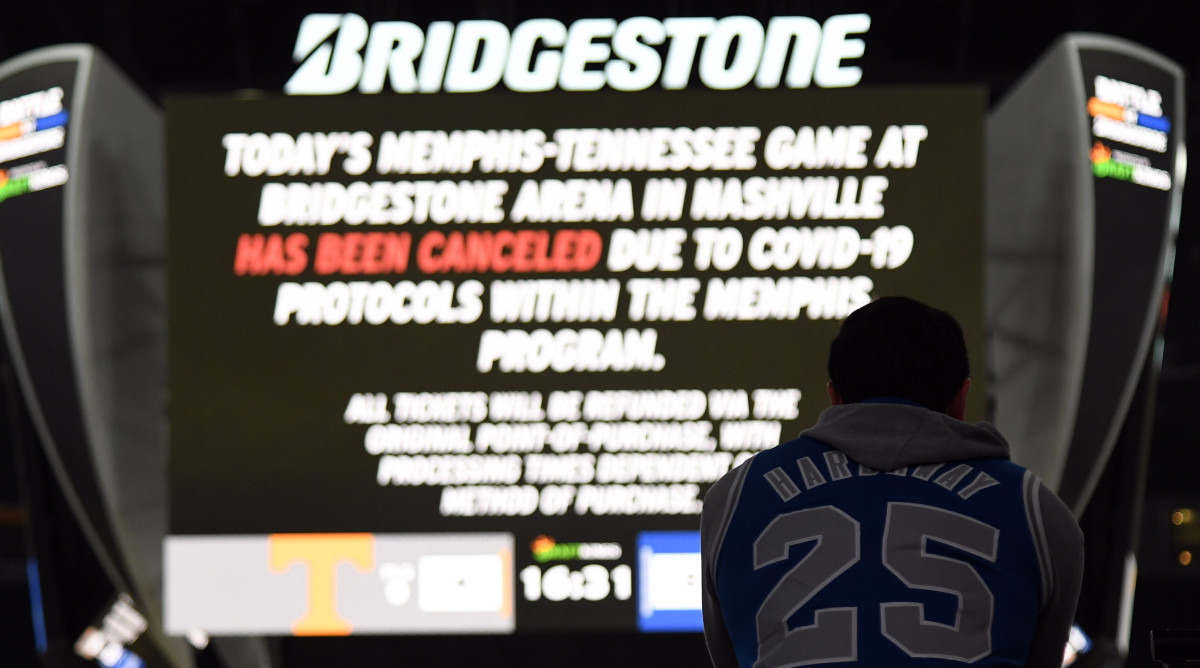
COVID-19’s latest surge, the fifth since the pandemic began 22 months ago, is wreaking havoc on college sports once again. The latest strain of the virus, the omicron variant, is spreading across the country at a busy time in the world of NCAA athletics. Conference basketball schedules are within a week or two of tipping off. Football bowl season is gearing up for its busiest stretch. And the College Football Playoff is on the docket, too.
So far, more than 120 men’s and women’s basketball games have been canceled by the coronavirus, according to figures tracked by the NCAA. Three men’s teams have had at least three games canceled already, including Jarmond’s Bruins. And at least two bowl-bound football teams, Miami and Texas A&M, have paused activities because of COVID-19 outbreaks.
The situation is serious enough that conference executives are exploring whether to reinstate coronavirus-related policies from last season. The NCAA’s own COVID-19 medical advisory group recently restarted its weekly Zoom calls, too, and is examining the possibility of resorting to 2020–21 COVID-19 guidelines.
Most college athletic departments curtailed weekly COVID-19 testing over the summer as they reached a high-enough vaccination level. At many schools, only unvaccinated or symptomatic athletes and coaches are regularly tested. Many programs also ended mitigation tactics such as wearing masks and social distancing.
“There are real conversations about going back into isolation and back into [regular] COVID testing from last year,” says Jeremy Cauwels, a member of the NCAA advisory group and the chief physician of Sanford Health in South Dakota.
While some suggest the latest surge may trigger the return of such protocols, the college athletics world—including some medical experts—believes the opposite: Protocols should be further relaxed in response to a strain that, while more contagious, has shown far less severity of illness than its troubling predecessor, delta.
In fact, NCAA leaders have been in conversation with officials from the CDC about adjusting the mandatory 10-day quarantine for young people who test positive, multiple physicians and college administrators tell Sports Illustrated. Their argument? Vaccinated young people are showing either no symptoms or very mild symptoms, and their symptoms are subsiding within two to three days.
“The question that needs to be asked is, if the risk of severe illness—hospitalization, death, dying—is not there, if we’re not seeing that, how is this different than the common cold?” asks Jeff Dugas, Troy’s team doctor and an orthopedic surgeon in Birmingham who chairs the Sun Belt’s COVID-19 advisory panel. “Do we need to be freaking out just because it is a variant of COVID-19? Do we need to apply the same rules or change the rules?”
It is a debate that's poised to further divide college sports along regionalized lines, indicative of the ongoing, 22-month fight in a fractured country.
“With omicron, the concern is not filling the hospitals with the sick, but one-third of the workplace not being able to go to work,” says Geoffrey Baird, chair of the department of laboratory medicine and pathology at the University of Washington. “Cases are doubling every two to three days. It’s taking over from delta.
“I’d call it worrisome and uncertain,” he continues. “Welcome to COVID.”
At the heart of the latest string of outbreaks across college sports is a familiar phrase: contact tracing. Contact tracing is the process by which health-care personnel search for people who are deemed “high-risk contacts,” defined as those within six feet for longer than 15 minutes of a person who tested positive.
Vaccinated high-risk contacts should be tested and, if negative, are allowed to continue participating but must produce at least one more negative test within seven days, according to CDC guidance. Those unvaccinated high-risk contacts must quarantine for at least 10 days.
Outbreaks are mostly happening in one of two ways: (1) enough unvaccinated or symptomatic athletes produce positive tests to trigger teamwide testing, which generates more positives; or (2) unvaccinated or symptomatic athletes produce positive tests resulting in a contact-tracing process that generates more positive results.
“The contact tracing piece is significant,” says Jarmond.
The same goes for the situation at Tulane. The private school in New Orleans has continued to regularly test all athletes. Both its men’s and women’s basketball teams have been shut down for more than a week.
Basketball naturally features more high-risk contacts than football, as it is played indoors and without a helmet. The sport also has a greater chance of a small handful of positives shutting down a team. Basketball teams range from 15–20 players.
“We have a number of symptomatic kids. If they are positive, you test everybody. It only takes one,” says Tulane athletic director Troy Dannen. “A lot of positives showing up in close contacts are asymptomatic.”
Contact tracing is made more complicated by the subjectivity involved. Whether politically or culturally motivated, schools hold disparate views on how to conduct this arduous task.
Some schools have completely stopped tracing high-risk contacts who are vaccinated, multiple administrators say. Others are following CDC guidelines.
“Everybody’s all over the board,” says Shane Lyons, athletic director at West Virginia and one of college athletics’ leading voices in NCAA rule-making. “It’s not uniform from health department to health department.”
Physicians even question the reliability and accuracy of contact tracing so deep into a pandemic, with an accessible vaccine and against a strain that is so mild and contagious. Omicron is transmissible enough that by the time a contact-tracing process is complete, viral spread through a target group has already happened, says Doug Ackerman, an associate athletic director at Oregon State who chairs the Pac-12’s medical advisory board and sits on the NCAA advisory group.
That said, tracing still represents an important step in slowing spread, he says. “We are going to see large outbreaks if we don’t take measures to stop the spread once we know it is there.”

Omicron is mutating at a rate—many times without a host even knowing—that it has recently become the most dominant strain in the U.S. It’s already so prevalent that Baird says contact tracing is rendered, at times, useless.
“When prevalence is low, it makes sense to contact trace,” he says. “When prevalence is so high and you’re getting closer to an endemic, the contacts you trace are likely to have had other contacts you might not know about.”
Meanwhile, dozens of asymptomatic, vaccinated athletes—some even with the booster shot—are enduring 10 days of isolation for having been around a positive person for at least 15 minutes.
It is another frustrating issue for coaches, athletes themselves and administrators—a topic that has sparked the dialogue between the NCAA and the CDC.
“Conversations are being had,” Cauwels says. “That’s the hard part—truly understanding when somebody is no longer infectious. The CDC doesn’t differentiate between a 70-year-old and a college athlete. That’s some of the work the NCAA is trying to do: Can we say there is a standard of safety that may be shorter for a vaccinated college athlete than your average 70-year-old?”
College sports aren’t alone. The NHL has paused its season. In the last week, several NFL games have been moved because of outbreaks among teams. The NFL, in fact, relaxed its surveillance testing policy to mirror the college model—testing vaccinated players less frequently.
College conference executives and medical councils have started seriously discussing restoring policies that deem COVID-19-impacted games “no contests” instead of forfeits. The Big 12 is finalizing plans to do so, sources tell SI. If a team doesn’t have available six scholarship players and at least one coach, games will be ruled a no-contest or the teams will work to reschedule them.
Several other leagues, including the Pac-12 and SEC, are exploring changing their policy. The NCAA basketball committee may need to examine its minimum number of required games (25) to advance to the Big Dance as well. The committee last year dropped that number to 13.
“We’ve got to dust off the playbook from last year. Now’s the time,” says Jarmond. “It’s not fair for teams to have to forfeit.”
Like the nation as a whole, college sports are regionalized. In the way that states control most COVID-19 protocols, leagues and schools have authority. The NCAA has little power outside of providing recommended guidance.
How different are conferences? The Pac-12 has recommended masking indoors. The SEC has not. That could change soon, though.
“The reality of returning to masking may be in our future,” says Chris Klenck, the head team physician at Tennessee who sits on the league’s COVID-19 medical task force. “Should this become something that is concerning, it may be we have to ramp up mitigation strategy.”
In a dash of positive news, omicron is so contagious and produces such mild symptoms that it may pass through the U.S. quickly, according to data from overseas. The strain is already subsiding in the population of South Africa, where it originated just a month ago.
Above anything, health experts still say vaccination is the answer to the bigger problem. Sure, vaccinated athletes are being infected and even experiencing some symptoms from omicron, but vaccination limits contact-tracing quarantine, suppresses severe symptoms and is a small piece of a grander puzzle to eradicate spread.
Schools are encouraging their athletes to get a third shot, the booster. Some are well ahead of others. Alabama, for instance, has had more than 90% of its players boosted, coach Nick Saban revealed earlier this week.
At Purdue, 80 of the 111 football players are scheduled to get their booster at an on-campus event Wednesday, says Doug Boersma, the director of sports medicine for the Boilermakers.
“They see the importance of getting vaccinated and not getting quarantined for contact tracing,” Boersma says. “I didn’t have to twist any arms.”
They are also preparing for what may be a spike from the holiday ahead. Athletes on teams participating in bowl games are normally allowed to travel home for Christmas break to spend the holiday with their family. Administrators fear that players will return having contracted COVID-19 with a bowl or playoff game days away.
The Alabama staff is giving each player what Saban terms a “care package” that helps explain how to remain safe over the holiday. Inside the football operations building, the Tide have implemented similar mitigation protocols to the ones used last year.
“Am I concerned?” Saban said. “I’m always concerned when there’s an issue out there.”
At Purdue, Boersma is prepared for a potential spike within the team post-Christmas. At the Music City Bowl site in Nashville, he’s reserved extra hotel rooms for those who must isolate or quarantine, and he’ll have COVID-19 test kits ready for those who are feeling symptomatic.
At Michigan, offensive lineman Andrew Stueber says that a “full team booster shot” is scheduled for Wednesday.
A handful of bowl games are in jeopardy already. Texas A&M and Miami, both paused for COVID-19 outbreaks, play in two separate bowls on Dec. 31: the Aggies in the Gator Bowl and Hurricanes in the Sun Bowl.
Bowl games represent significant financial paydays for conferences. Each participating school gets a bowl payout that is sent to the conference and then distributed among the league. The Gator Bowl, for example, pays out $5.35 million. If a bowl game isn’t played, the check isn’t delivered.
If a team can’t play in a bowl game because of COVID-19, there are no possibilities of a replacement like last year, says Nick Carparelli, the bowl season executive director. Carparelli is “very optimistic” that all bowl games will be played.
“College football is unique in that it is the largest roster in the sport,” he says. “I think teams can withstand a couple of cases. These teams have earned their way into bowl games and they want to play them.”
COVID-19 testing protocols at both bowl sites and CFP games are determined by the teams and conferences. However, those coming into contact with CFP semifinal staff and players at the Cotton and Orange bowls are required to be vaccinated, including media and anyone else on the sideline.
In response to rising cases, all media access at the CFP will now be held virtually, and attendance at events at game sites will be optional for athletes. Bowls and semifinal sites could make further adjustments moving forward if community spread warrants.
In the meantime, scientists continue to plow away at turning a pandemic into an endemic, a disease that regularly lives among a population, such as the flu.
The world is “close” to reaching that point, physicians say. One last hurdle is nearly crossed, says Cauwels. Oral therapeutics to treat COVID-19 are in the process of being approved by the FDA. That could come by spring.
“Then we have to figure out how to move through life with the virus,” he says. “The question is, if everybody on a team is vaccinated completely, do you test and worry about the virus breaking out if you know everyone on the team is very unlikely to have a severe illness?”
Until that question is answered, until an endemic arrives, college sports continue to navigate an uncertain world—again.
“There was the feeling that we’ve seen the worst of this,” Jarmond says. “We’ve learned quickly that we’re not out of this thing yet.”
More College Football Coverage:
• Bowl Game Watchability Rankings
• Meet the Football Guru Who Helps Guide Alabama (and Michigan and Georgia...)
• Cade McNamara, World-Beater? He Thinks So.
