Big Ten Medical Report Details Serious Cardiovascular Concerns From Experts
BLOOMINGTON, Ind. — Recent studies on myocarditis and other cardiovascular concerns related to the COVID-19 virus and its unknown risks to college athletes playing sports this fall likely played a big role in the Big Ten's decision to postpone the football season
In a five-page document obtained by Sports Illustrated Thursday, the Big Ten put out a bulletin about "Cardiovascular Evaluation and Recommendations for Returning to Full Practice and Competition Following COVID-19 Infection/Testing Protecting the Safety of Big Ten Student Athletes," and the numbers of people who have had heart issues after COVID are shockingly high.
___________
- RELATED STORY: Two Indiana cardiologists explain myocarditis and its effects on athletes and others. CLICK HERE
___________
The bulletin is dated Aug. 11, which is the same day the Big Ten postponed its fall sports. It was prepared by three cardiologists — Lawrence D. Rink, who works with Indiana's athletic department, Michael S. Emery from the Cleveland Clinic, and Eugene H. Chung from the University of Michigan.
The document states, "While there is general agreement among sports cardiology experts to increase the level of scrutiny for potential cardiac involvement in athletes who have or are recovering from COVID-19, there are conflicting recommendations with regards to which athletes to test, the extent of cardiac testing, and convalescent periods."
The report referenced a study conducted from 100 recently recovered patients from COVID-19. The median age was 49 years old with the median time interval between COVID-19 diagnosis and cardiac MRI of 71 days. The results were that 67% of patients recovered at home rather than needing hospitalization, including 18 asymptomatic patients. High sensitivity Troponin — a sensitive marker for cardiac cellular injury — was detected in 71% of the patients and cardiac MRI revealed evidence of cardiac inflammation and/or scarring in 78% of the patients.
"These studies demonstrate that cardiac injury can occur in less ill and even asymptomatic people with COVID-19 and requires due diligence on cardiac assessment and thoughtful consideration for longitudinal care. While these studies may not be completely applicable to university athletes, we must exercise extreme caution given the level of heightened concern for myocardial involvement and the potential implications of sudden cardiac death in athletes with myocarditis."
Quick turnaround in decision to play
Reports like these may have swayed decision-makers at the highest level of the school's 14 universities and in the Big Ten offices. Just six days after announcing a new fall schedule, they postponed the entire season, raising consternation among players, coaches and fans alike.
After the Big Ten announced that it was postponing the fall football season, league commissioner Kevin Warren was asked about the emerging information of myocarditis, and he said the uncertainly over its affects on athletes warranted further conversations.
'There has been a lot of discussion about myocarditis, so there has been discussion as of late," Warren said. "That's not the primary reason. All of those items from a medical standpoint, you have to consider.
"I know there's been a lot of discussion about that, but overall when it comes down to it, it's just the litany of things that created this state of uncertainty that we need more clarity on from a health, wellness and medical standpoint."
Within the document is a return-to-play algorithm for the assessment of cardiac involvement. It states that the Big Ten's actions are "more conservative than the current American College of Cardiology (ACC) recommendations, specifically in regard to testing of asymptomatic athletes and additional convalescent time before an athlete could practice/compete."
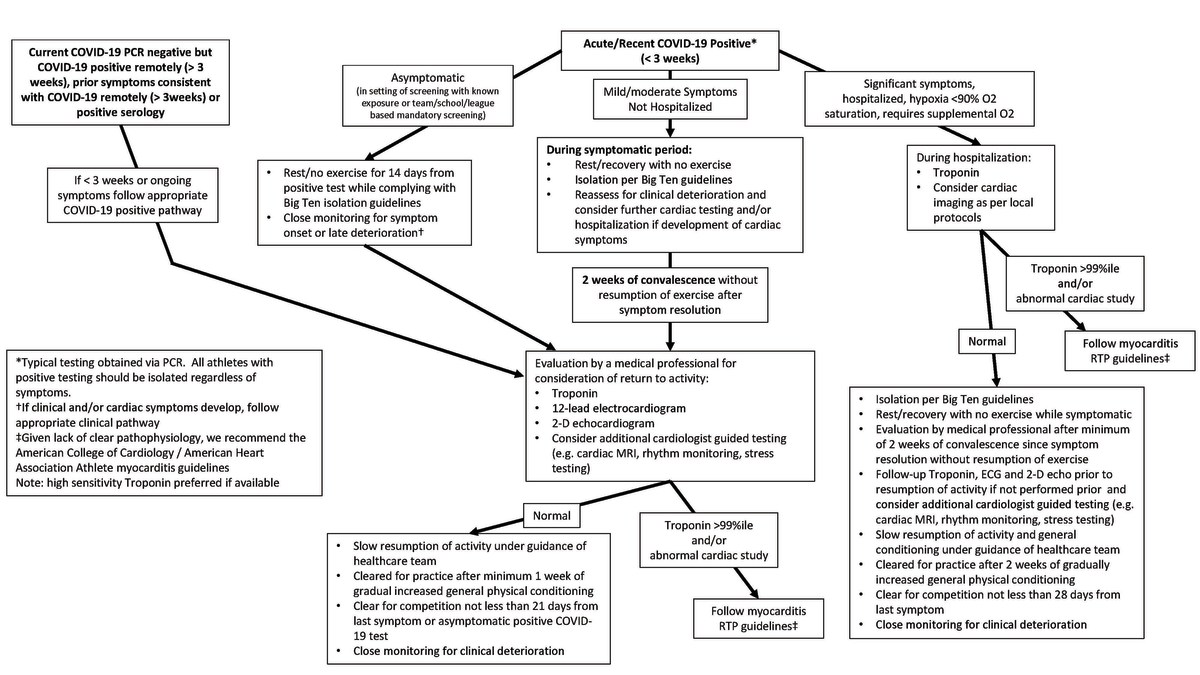
It clearly states that these guidelines are not meant to be a comprehensive guide to diagnosing COVID-19 related myocardial involvement/myocarditis. Rather, "they provide a framework for raising suspicion of possible involvement and serve as a guide to return-to-play in those not specifically found to have cardiac involvement."
According to the report, here are the current cardiac recommendations for athletes who are asymptomatic and athletes who are very symptomatic:
1. Asymptomatic and mildly/moderately symptomatic COVID-19 athletes:
a. Follow isolation guidelines Listed in the Big Ten playbook and Big Ten bulletins. Release from isolation does not indicate clearance for exercise.
b. Athlete should refrain from exercise except for activities of daily living (ADLs) for 14 days after the diagnosis regardless of symptoms (this may be concurrent with period of isolation).
c. Athletes with symptoms should have a 14-day period of convalescence after symptom resolution with no more than mild exertion beyond ADLs.
d. All athletes should have an ECG, comprehensive echocardiogram and troponin — high sensitivity troponin preferred if available — prior to anything other than mild exercise after completion of recommended isolation period. Viral-induced myocardial involvement that could manifest on an ECG include pathological Q waves, ST segment depression, new diffuse ST segment elevation, and/or T-wave inversion.
e. If any of these tests are abnormal, additional testing should be performed under the guidance of a consulting cardiologist in conjunction with the sports medicine physician that is knowledgeable about cardiac issues and exercise. Additional testing to be considered are cardiac MRI with contrast, rhythm monitoring, stress testing and additional laboratory studies. It is strongly recommended that cardiac MRI with contrast be performed in the initial assessment of any screening abnormality in conjunction with experts in their application and interpretation. Some university sports medicine departments may wish to include this additional testing in all COVID-19 positive athletes.
f. Athletes cannot resume physical activity until being cleared by their sports medicine physician in consultation with cardiology who have reviewed all of the pertinent studies and believes there is no active cardiac involvement or symptoms that would put the athlete at risk. Signs and symptoms that might indicate cardiac involvement include excessive dyspnea on exertion, hypoxia, palpitations, unexplained tachycardia, chest discomfort, excessive fatigue, near-syncope or syncope.
g. After cardiac clearance is obtained, the athlete can begin a minimum of 7 days of gradual increase in physical conditioning/training under medical supervision. If this conditioning period goes well, the athlete can be cleared for full practice and competition.
h. The minimum time frame to resume full practice/competition should be a minimum of 21 days after diagnosis if asymptomatic or after the resolution of symptoms which should include at least one week of gradual resumption of exercise training.
2. Severely symptomatic (requires supplemental oxygen, prolonged symptoms) or hospitalized athletes:
a. Follow the above testing, isolation and convalescence protocols.
b. If hospitalized during acute illness and there is evidence of significant myocardial involvement, these athletes will need to be dealt with on an individual basis in consultation with cardiology specialists and team physicians.
c. Initial evaluation by the sport medicine physician should include a thorough review of all prior testing including those that may have been obtained in the hospital or emergency room. Consultation with specialists as appropriate should be considered.
d. The athlete without cardiac involvement will undergo a 2-week convalescence period after all symptoms have resolved.
e. During the convalescence period, perform ECG, echocardiogram and troponin (high sensitivity troponin is preferred if available) along with other appropriate testing as indicated if not done prior or level of suspicion of cardiac involvement is present. Signs and symptoms that might indicate cardiac involvement include excessive dyspnea on exertion, hypoxia, palpitations, unexplained tachycardia, chest discomfort, excessive fatigue, near-syncope or syncope.
f. Following the 2-week convalescent period from symptom resolution with all testing negative, no concerning symptoms and cleared by the sports medicine physician (in conjunction with cardiology consultation if appropriate), the athlete may begin a medically supervised conditioning program for their sport under the direction of the health care team/trainers.
g. Athlete can resume full training and competition 14 days after gradual increase in supervised conditioning/exercise training (assuming all went well and was well tolerated by athlete), no less than 28 days after symptom resolution, and cleared by appropriate sports medicine physician.
The report also states that if an athlete has abnormal cardiovascular testing, they will not be cleared for participation until all tests return to normal and have been cleared by the consulting cardiologist and sports medicine physician who is very familiar with cardiac abnormalities.
Different perspectives from each conference
As of now, the Big Ten and Pac-12 are the only two Power 5 conferences to postpone fall sports. The SEC, ACC and Big 12 have all announced they plan to move forward as of now, and that they have a different conclusion to the medical reports they have reviewed.
“Reasonable people can disagree on it, and the Pac-12 and the Big Ten are seeing much of the same information that we’re seeing,” Bob Bowlsby, the Big 12 commissioner, said after his league released its football schedule on Wednesday morning. “But our board believes in our scientists and has come to a conclusion that’s different, and so have the leadership of the SEC and the ACC.”
Greg Sankey, the SEC commissioner, said in an interview that the moves by other leagues, including smaller conferences, were “informative, not determinative.”
On Thursday morning, the NCAA's chief medical officer and two primary infectious disease advisers said they don't think fall sports should happen.
"I feel like the Titanic. We have hit the iceberg, and we're trying to make decisions of what time should we have the band play," said Carlos Del Rio, who serves on an NCAA COVID-19 advisory panel.
“We need to focus on what's important. What's important right now is we need to control this virus. Not having fall sports this year, in controlling this virus, would be to me, the No. 1 priority."
